Breast cancer first touched Philippa Decuir’s life when her sister Mabel was diagnosed with the disease in Rwanda in 1987. Breast cancer was stigmatized then. Locals commonly believed it was caused by a curse, Decuir recalled.
“When she was struck by the disease, she didn't even know what it was,” Decuir said of her sister. Mabel died at 38 years old, with no access to treatment in her home country.
Decuir herself was diagnosed with breast cancer less than a decade later while living in Houston. She was treated quickly and cured after an early detection. The stark difference between her cancer care in the U.S. and what her sister was afforded in Rwanda inspired her to start the Breast Cancer Initiative East Africa (BCIEA) in 2007.
01 / 03
There is much work to be done to improve treatment access for cancer patients in Rwanda—and countries across Africa. Decuir’s organization is one of several partners that Hurone AI, an Amazon Web Services (AWS)–powered medical technology startup, has teamed up with to improve patient outcomes in the country.
Rwanda now has multiple cancer treatment facilities and active educational campaigns for women, thanks to organizations like Decuir’s and leadership from the Rwandan government. But the small number of oncologists in Rwanda means that patients still have limited access to care.
A country that has roughly the population of Pennsylvania—about 13.5 million people—Rwanda has fewer than 15 oncologists. Across sub-Saharan Africa, there is roughly one oncologist for every 3,200 cancer patients. By comparison, the U.S. ratio is about one oncologist for every 300 patients. Even with oncology care, many Rwandan patients must make arduous commutes to medical facilities, and they wait until symptoms are dangerously severe before reporting them.
 The Rwanda Cancer Treatment Centre in Kigali.
The Rwanda Cancer Treatment Centre in Kigali.Democratizing access to care
Hurone AI is setting out to solve the access problem for patients—while also making life easier for doctors. The Hurone AI team created a digital application that allows doctors and patients to communicate frequently and easily through auto-generated text message prompts about symptoms and side effects.
Last November in Rwanda’s capital of Kigali, Hurone AI launched initial patient tests of the messaging system. They call it “Gukiza,” which means “to heal” in Kinyarwada, one of four languages commonly spoken in Rwanda.
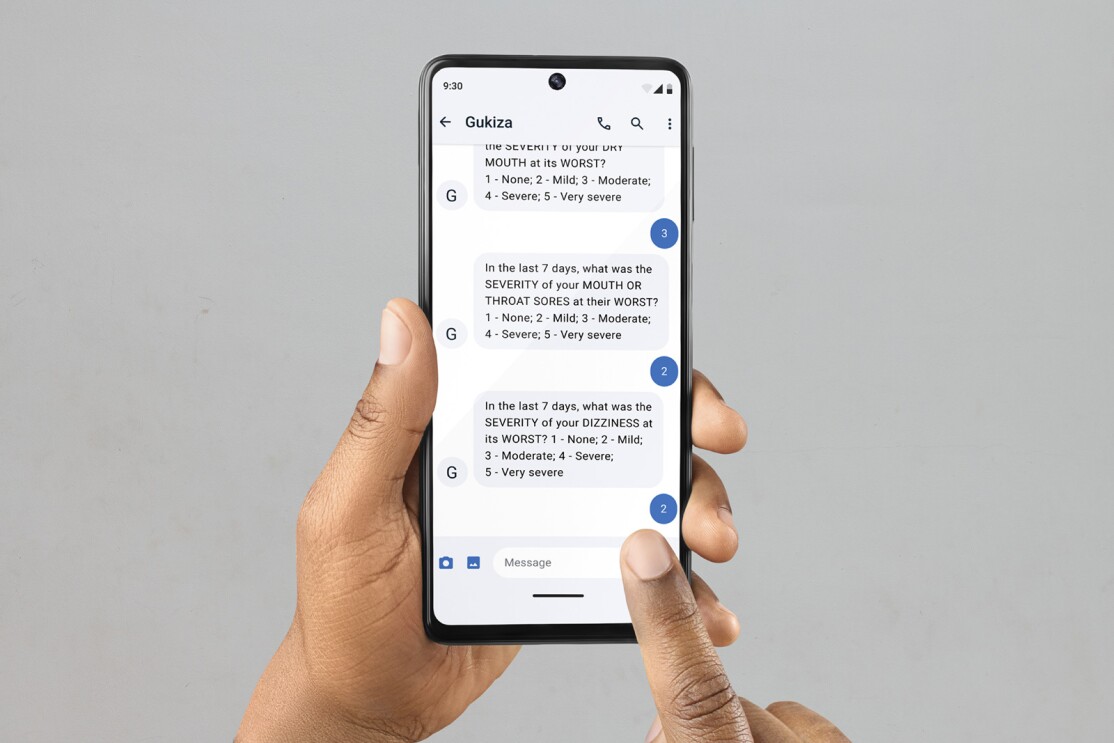 Text message prompts about patient symptoms and side effects on the Gukiza app.
Text message prompts about patient symptoms and side effects on the Gukiza app.The application will serve as a valuable tool for local oncologists who are spread thin. Through the web app, doctors will be able to adjust treatment plans quickly if a patient reports problematic side effects. If new symptoms are reported through a patient’s text messages, doctors will be able to treat those remotely or schedule an in-person appointment, if necessary.
“We can design a system that can understand, ‘Okay, this person has the symptoms of dehydration,’” explained Hurone AI Founder Kingsley Ndoh. “And so, the AI can help craft that message, and one of the care team members will just edit and send.”

As testing continues and doctors gather data on everything from reported side effects to the efficacy of ongoing treatments, they also expect to be able to predict ideal treatments for future patients through artificial intelligence (AI).
Moving from scrappy beginnings to cloud technology
The success of this work relies in large part on data—and the team’s ability to acquire, store, and analyze it.
“To design a lot of these machine learning models, you need big data, and you need reliable cloud computing that can help you reach millions,” Ndoh said. “You need a very reliable cloud that is doing it already.”
In March 2022, Hurone AI was selected as one of more than 90 organizations to receive cloud credits—an allotment of free AWS services—as part of the AWS Health Equity Initiative. The initiative, a three-year, $40 million commitment from AWS, is rooted in the belief that health outcomes should not depend on socioeconomic status, race, or ethnicity.
“Cloud technology can help address inequities in global health to expand access to the services people need to live longer, healthier lives—no matter who they are or where they live,” said Maggie Carter, director of global social impact at AWS. “Through the program, we look forward to helping Hurone AI and other organizations worldwide use the power of cloud computing to advance health equity and improve health outcomes.”
Hurone AI and the AWS Health Equity Initiative were recognized by the White House last December as programs that demonstrate a promise to reduce the burden of cancer in Africa—part of President Joe Biden’s Cancer Moonshot effort.
Providing a localized approach, with potential to scale
The Hurone AI team is staying laser-focused in its early stages, launching its pilot program with about 200 breast cancer patients in the Kigali region.
But the team’s ambitions go far beyond this small group in Rwanda. This year, they are laying the groundwork for a similar pilot program in South Africa.
They also expect to learn more broadly about cancer’s impact on African populations, which are often overlooked in medical research.
“Most of the organized clustered data that exists in this world is for the Western world,” said Lior Romanowsky, Ndoh’s technical partner with Israel-based company called Spartans. “In Africa, it's definitely a problem.”
Romanowsky, Ndoh, and the Hurone AI team plan to aggregate and chart models across demographic data, clinical data, and patients’ family histories. Their goal is to be able to predict both diagnoses and treatment outcomes based on their data analysis.
Ultimately, the doctor-patient messaging system could be created and localized for any population where medical facilities are hard to access. And the data analysis from African countries could become useful for all patients of African descent—including patients in the U.S.
“Our long-term vision is to leverage culturally sensitive technologies that Hurone AI is building to improve treatments for patients, improve treatment strategies for doctors, and to ultimately improve outcomes for everyone,” said Ndoh.
Trending news and stories
- Amazon’s new AI experience helps sellers visualize and grow their business in real time—here's how it works
- Inside Gen AI's split-second sprint from question to answer
- Amazon offers free returns with no box, tape, or label needed
- Amazon’s S-team: Meet the 28 members who make up our senior leadership team